It's been years since we've posted on the blog, but I thought I'd do a quick update.
Our now 6-year-old daughter has been doing maintenance doses of peanut butter every day since she graduated in 2015. Most of the time, it's no big deal... it was hard to get her to eat it at first, but we've got a system down.
She gets her peanuts directly after dinner since we generally can observe a couple of hours of calmness afterward. But she has to have them at least an hour before she goes to sleep or her hormone levels which change at that time may cause a reaction. We mix a 1:1 ratio of peanut butter to powdered sugar, scoop it into balls and put chocolate chips studded around it. She has gotten good enough to just eat her two 1/2TBS peanut butter ball in one bite. Then she washes her hands and we're done! We have loved being able to send her to school without worrying about lunch, treats, etc. It's wonderful!
There have been a handful of nasty reactions, however. The first happened probably about 6 months from her graduation when she took a warm bath a couple of hours after her dose. We were doing peanuts in the morning back then. After her bath, she hopped out and was chilly. Almost immediately she was covered in hives and coughing. I gave her oral medications, but her coughing and itching were so intense and the crying freaked me out. I ended up giving her the Epipen for the first time (and last to date). Her oral medications may have worked, but I didn't want to risk not giving the epinephrine.
She's had other reactions after that as well, usually after an hour or so of eating peanuts and then jumping on the trampoline, coming inside from playing in the snow or doing something that really raised her body temperature. That's partly why we've moved her dose time to the evening. There's less physically going on during that time, so she stays cool and calm.
Her recent blood work had her overall anti-peanut antibodies down in the 20s! That's a huge difference from >100!
We have had a wonderful experience with OIT so far, and while we aren't happy that our 1-year-old daughter also has a peanut allergy, we are hopeful that she can have just as good an outcome.
Girl vs. Peanut
Wednesday, February 7, 2018
Wednesday, November 11, 2015
Peanut IgE results - Before and After Oral Immunotherapy
Since I know there are a number of people who follow this who are knowledgeable about and interested in the peanut IgE labs, this one is for you:
Quick recap of our girl’s story:
- Severe peanut allergy.
- Told in no uncertain terms from her original allergist to have strict avoidance of peanuts and that there was a “100% chance” that any exposure to peanut would cause a major and potentially life-threatening reaction.
- High peanut IgE levels (details below).
- Introduced to peanut Oral Immunotherapy (“OIT”) done by Dr. Douglas Jones at Rocky Mountain Allergy in Layton, Utah.
- We went through ~6 months of “Oral Immunotherapy” (starting with insanely tiny twice-daily doses of peanut protein and very gradually increasing the dose over 6 months until she ate 24 peanuts all at once with no reaction and graduated).
- Now she’s on “maintenance” twice-daily dosing of 8 peanuts.
- …And now here we are. We just got her labs drawn again. Here are the results:
In short, yes, the labs still look very scary from your classic school of thought on allergy IgE interpretation, but two point to remember:
- The labs have all actually improved since she’s completed oral immunotherapy.
- Remember that even with these labs, she’s eating at least 8 peanuts twice a day, and yet the IgE levels have gone down, and she’s doing just fine :)
And not that it matters much, but I’m still very much enjoying peanut butter in the house. Actually, I had some on my waffles this morning :)
Thanks again to Dr. Jones and his staff!
Wednesday, May 13, 2015
Peanut OIT Graduation! She eats peanuts now!
And now some explanation, of what exactly happened today, and what that means for us now.
WHAT HAPPENED FOR THE GRADUATION:
 Well, clinically, nothing too out of the ordinary. We've been coming to the clinic each week on Wednesdays to escalate her dose. This was pretty much just like those, except for the notable fact that this was the last one of the weekly visits. That, and the fact that she's never eaten so many peanuts in her life at one time before, and she did just fine. The "graduation" dose was 24 peanuts. Being a four-year-old, she takes her time eating, and it's a lot faster when it's in the form of something other than a plain ol' peanut, so she actually had the equivalent of 24 peanuts in peanut M&M's (all yellow as that's her favorite), two plain peanuts, and peanut butter.
Well, clinically, nothing too out of the ordinary. We've been coming to the clinic each week on Wednesdays to escalate her dose. This was pretty much just like those, except for the notable fact that this was the last one of the weekly visits. That, and the fact that she's never eaten so many peanuts in her life at one time before, and she did just fine. The "graduation" dose was 24 peanuts. Being a four-year-old, she takes her time eating, and it's a lot faster when it's in the form of something other than a plain ol' peanut, so she actually had the equivalent of 24 peanuts in peanut M&M's (all yellow as that's her favorite), two plain peanuts, and peanut butter.
She ate it. We waited. No reaction as usual. Graduation.
That's it.
The postscript and gee-whiz on that story is that Dr. Jones told us that our girl was probably the youngest patient he's had graduate from peanut OIT (He's had younger patients graduate from other allergy treatments -- Milk, egg, etc., but not peanut). She just recently turned four years old, for future reference.
 And as niceties, at graduation, she was awarded with a graduation certificate and some free kids meals at Texas Roadhouse (which notably is probably the one restaurant that is the farthest from peanut-free you can get as you may have noticed).
And as niceties, at graduation, she was awarded with a graduation certificate and some free kids meals at Texas Roadhouse (which notably is probably the one restaurant that is the farthest from peanut-free you can get as you may have noticed).
WHAT DOES THIS MEAN FOR US NOW?
 Well, the biggest and best change is that she's now free to eat peanuts! We don't have to check food labels for peanut contamination or peanut ingredients. We don't have to worry that some kind sharing 4-year-old is going to share something with her that will be fatal. Heck, if someone is having a snickers bar, she can have some too.
Well, the biggest and best change is that she's now free to eat peanuts! We don't have to check food labels for peanut contamination or peanut ingredients. We don't have to worry that some kind sharing 4-year-old is going to share something with her that will be fatal. Heck, if someone is having a snickers bar, she can have some too.
And best of all, we don't have to worry about her safety from hour-to-hour and we don't have to always be anxious about if she's safe or not.
THAT is a good feeling, my friends.
 Now... a couple of caveats. :) Yeah, yeah, it's not all fluffy clouds, daisies and marshmallows... (but it's pretty darn close...). Here's how it goes for us from this point. She will need to take a maintenance dose of 8 peanuts (or equivalent) morning and night for 6 months. After that, I believe she switches to a final maintenance dose of 8 peanuts per day just once per day. In a while, we will be taking her to get some labs drawn, and I'll post the "before and after" numbers for those of you who are interested. I'm not sure what to expect from the lab numbers. If I remember right, I think Dr. Jones says the IgE levels raise with this, but I really don't know if that's just an initial raise when the treatment is started and then they drop again? I just don't know. And frankly, I don't really care. Whatever the lab work says, it doesn't change the fact that she can eat them by the handful now and handle it just fine. I do remember Dr. Jones talking to us at the beginning of this treatment telling us that he had seen a bunch of times when a patient's peanut IgE level were sky-high, off-the-charts, and the person was eating peanuts by the handful no problem. That's what matters, after all.
Now... a couple of caveats. :) Yeah, yeah, it's not all fluffy clouds, daisies and marshmallows... (but it's pretty darn close...). Here's how it goes for us from this point. She will need to take a maintenance dose of 8 peanuts (or equivalent) morning and night for 6 months. After that, I believe she switches to a final maintenance dose of 8 peanuts per day just once per day. In a while, we will be taking her to get some labs drawn, and I'll post the "before and after" numbers for those of you who are interested. I'm not sure what to expect from the lab numbers. If I remember right, I think Dr. Jones says the IgE levels raise with this, but I really don't know if that's just an initial raise when the treatment is started and then they drop again? I just don't know. And frankly, I don't really care. Whatever the lab work says, it doesn't change the fact that she can eat them by the handful now and handle it just fine. I do remember Dr. Jones talking to us at the beginning of this treatment telling us that he had seen a bunch of times when a patient's peanut IgE level were sky-high, off-the-charts, and the person was eating peanuts by the handful no problem. That's what matters, after all.
Further caveats: I don't know how long this lasts, but yes, we've been told to still keep her epi-pen with her just in case. Frankly, even if he didn't tell us to do that, I'd probably still want to do it. It can't hurt, and it might help. So yes, she'll still have that little accessory tagging along with her.
But ladies and gents -- she's safe. That's why we started this thing. That's why we researched this thing up and down to see what we could find in the medical literature about it, and made the resolute decision that we were going to pursue this.

 A big thank you to the many friends/neighbors/family members who have helped us do this. Thank you to my sister Christa for alerting us to the existence of this clinic in the first place. Thanks to you who made an extra effort to have only peanut-free foods at social/family events before we started. Thank you SO MUCH to the friends/neighbors/family who watched our baby while Katie took our 3-4 year old to do these treatments every week. And of course, a huge thank you do Dr. Jones and his staff at Rocky Mountain Allergy for making this still very rare chance available to his patients. It's a risk for them to be breaking the common allergy/immunology clinic inertia, going very much directly against the mainstream medical train of thought with these patients who have severe allergies. They are daring to actually *treat* the condition and not just collect patient fees, tell patients to avoid peanuts, and then blame noncompliance with the treatment when "strict avoidance" doesn't turn out to work in a world filled with peanut products.
A big thank you to the many friends/neighbors/family members who have helped us do this. Thank you to my sister Christa for alerting us to the existence of this clinic in the first place. Thanks to you who made an extra effort to have only peanut-free foods at social/family events before we started. Thank you SO MUCH to the friends/neighbors/family who watched our baby while Katie took our 3-4 year old to do these treatments every week. And of course, a huge thank you do Dr. Jones and his staff at Rocky Mountain Allergy for making this still very rare chance available to his patients. It's a risk for them to be breaking the common allergy/immunology clinic inertia, going very much directly against the mainstream medical train of thought with these patients who have severe allergies. They are daring to actually *treat* the condition and not just collect patient fees, tell patients to avoid peanuts, and then blame noncompliance with the treatment when "strict avoidance" doesn't turn out to work in a world filled with peanut products.
It should also be noted that the shirt she wore today -- her choice. Not ours. :)
Labels:
Allergy,
Anaphylaxis,
Medical,
OIT,
Oral Immunotherapy,
Peanut,
Peanut Allergy,
Peanut Allergy Treatment,
Peanut IgE,
Progress,
Success
Location:
Layton, UT, USA
Friday, April 10, 2015
Q&A Part 3: Home Dosing
1. Q: How does dosing at home work?
A: When you’re home you give the appropriate dose (it’s like a prescription) of the allergen twice a day about 12 hours apart (there’s a 9-15 hour window). We usually dose in the morning between 7 and 9am (early on the days she has preschool), and then dose again somewhere between 6 and 8pm, depending on how early our daughter needs to go to bed. This has been one of the hardest things for us because she’s young enough that sometimes she naps and sometimes she doesn’t. It’s hard when our appointment is at 10:00 am, with her escalation dose around 10:30am – so we can’t give her medicine until 7:30pm at the earliest, but bedtime is 7:00pm if she hasn’t napped! If I had to do this again I would either wait until she wasn’t napping at all and going to sleep around 8 or live closer so that I could get to the office earlier.
A: There are actually quite a few which were hard to remember at first, but have gotten much easier since we do it twice a day.
 A: Changes as you go – and this is specific to peanut.
A: Changes as you go – and this is specific to peanut.
- Probiotics (the dose depends on the kid) – this is to help prevent stomach upset which is the most common side effect. Our kiddo has not complained of stomach problems, but she’s been on a probiotic since we started OIT. It’s another “medicine” that has become a part of our day at morning and at night. We started with the more expensive brand, but changed to the cheaper brand and it doesn’t seem to have affected her.
- Rest – She’s supposed to rest a half hour before and 2-4 hours after each dose. Um… yeah right! She just turned 4! But she’s pretty good to sit and play with the iPod, or watch a movie, or do “light” activity with me. I try to get her resting time in before preschool at 9:15, but we frequently cut it close (but she hasn’t had a problem yet). Increased activity increases the heart rate and temperature, which can activate the immune system to respond to the allergen more readily, which is why they strongly suggest resting.
- Eat 15 minutes to 1 hour before. This is harder than it sounds. My kids don’t eat straight away in the morning – we all have what we call “sleep inertia.” So getting her to eat before 7am so that she can be dosed, rested, and ready for preschool at 9:15 is harder than it sounds, hence why we “cut it close.”
- No sleeping for an hour afterwards. Again this is easier said than done when your kid goes to bed at 7:00pm. We have to take snacks and her dose anytime we are going to be out for the evening. It’s not difficult, but it is a nuisance.
- No dosing after 9pm. This is because cortisol levels change as we get ready to sleep. This one has never been a problem for us since she’s always dosed pretty early, but I wonder if cortisol levels are different for kids her age……
- Missed dose or not within the 9-15 hour window or outside any of the above rules – you call the office during office hours, or call/text Dr. Jones when they are closed. There are specific instructions for if this happens so that you don’t run the risk of overdosing beyond what can be tolerated. We have been fortunate so far to only have to text a few times, but when we do, the response time is pretty prompt.
 A: Changes as you go – and this is specific to peanut.
A: Changes as you go – and this is specific to peanut.- Liquid – they dissolve a tiny amount of peanut flour into Kool-Aid and you administer it with an oral syringe. Each escalation dose increases either in amount or concentration.
- Flour (50, 100, 250, 500mg) – we mixed it into yogurt, applesauce, or pudding. She preferred yogurt and applesauce! I was sure she’d love it in the pudding… but nope.
- Whole, roasted peanuts (1 at a time until 8, 10, 12, 24). We started out by giving her chocolate chips with her peanuts, but after a few weeks we could use M&Ms or peanut butter. If the patient has multiple allergies you have to be careful about what you use (peanuts in the shell, no M&Ms because of cross contamination, flavored peanut butter, etc.).

- The Office will provide all the liquid doses, the flour, and the first 2 weeks of whole peanuts where they have to be measured carefully. After 3 peanuts, the size variation is negligible, so they have you bring your own peanuts, M&Ms, or peanut butter.

A: This is our worst fear, right?! We’ve been blessed so far to have had only very minor reactions if any. She’s had a couple random hives on her face, but they’ve always popped up hours after her dose, so I can’t even be positive that it was the peanuts and not some other thing. Most reactions occur within one hour of dosing (if I remember correctly), which is why we are supposed to watch her closely for that first hour (that’s also another reason why they shouldn’t go to sleep within an hour of dosing). We have a “Home Emergency Plan” typed up and taped to the inside of our cabinet by the phone and fridge so that we can find it quickly if a reaction should take place.
- Mild Reaction – (ie. A hive). Report it to the office before the next dose. Watch it carefully to make sure it isn't progressing into something worse. Hopefully the body will resolve it quickly.
- Moderate Reaction – (ie. Hive progresses into a full body rash). If the mild reaction progresses or worsens, then call the office immediately. Before we started, the only medications we had were Benadryl and the epi-pen. When we started this treatment, they gave us prescriptions for 3 other medications (Zantac, Prednisolone, and Allegra). If she has a moderate reaction and the Dr. says to, we would give all three of those medications at a certain dosage, as prescribed. We had to do the Zantac alone once because she threw up… but it was precautionary, as we were pretty sure it wasn't due to the peanuts. Some parents have these three meds with them all the time just as they do the epi-pen. We chose to leave them at home since that is where we are almost always when she is being dosed and for the resting periods when a reaction is most likely to occur.
- Severe Reaction – (ie. Anaphylaxsis -this is when multiple body systems are involved. Hive + Throwing up. Or Hive + Throwing up + Swelling.) This is the scary stuff that we are so grateful to have yet to experience it (and hope never to). All care givers of kids with food allergies should know what to do in this instance:
- Give the epinephrine!
- Get to the Emergency Room (not insta-care)!
- Call Dr. Jones.
- Give the 2nd epi-pen included in the pack if needed on your way.
- If in doubt, give the epi! And yes, during this treatment, always have an epi-pen with the child!
One more Q&A to come; when we are done we’ll let you know what the maintenance is like, what graduation day is all about, etc. Any other questions you want us to address?
Monday, March 16, 2015
Q&A Part 2: Dr. Office Peanut OIT
This is
purely from our perspective, our experience. These details are specific to our
situation, but would probably be very similar to any other patient looking in
to doing oral immunotherapy (OIT)
through Dr. Jones at Rocky Mountain Allergy, Asthma, and Immunology (RMAAI).
through Dr. Jones at Rocky Mountain Allergy, Asthma, and Immunology (RMAAI).
1.
Q: What’s are the office visits like?
A: The first appointment is just to discuss things
– you as the parent (or patient) decide if this is something you really want to
commit to. The whole process takes about six months. Possibly more depending on if things happen
to throw off the schedule (illness, more severe reactions, etc.). They will order
either skin or blood tests to determine the extent of the allergy (we did blood
tests, since we had our documented test results from our previous doctor in
hand for this visit). The first day which I've already described is the
longest. From then on, it means coming
back into the office every week for an "escalation dose" -- meaning
that's where they increase the dose to a new level and monitor for an hour that
there are no problems with the new level of peanut protein in the system. What does this look like in actual
practice? Every week you come to the
office and (1) check in, (2) have the physician or one of his colleagues do a
physical assessment and vitals check, (3) take the new increased dose with the
nursing staff, and (4) sit around in a room in the office for an hour doing
whatever it is you do to entertain a 3 year old (books, trains, Hungry Hungry Hippos,
puzzles, and of course everyone brings their electronic gadgets too). Parents get to chat and talk about all the
things that no one else really understands about the best epi pens, how to
survive at family functions, what you tell their teachers, and so forth. A
reaction to the newly escalated dose is much more likely to happen within the
first hour which is why you get to wait. If there is no problem with the new
dose, they send you on your way with enough of the same dose to do at home for
another week. The dose then escalates again
the following week. No, you are never
increasing the dose at home by yourself, and you still always have the epi-pen
and other meds handy.
2.
Q: What’s the first day of OIT like?
A: The first day of actual treatment is LONG! Check out
Brett’s post about our first day here. You start out taking a teenie tiny dose
of the allergen, then it is doubled every 15 minutes for 5 hours. Brett did the
math and on that first day Lindy consumed 7.6
100ths of a peanut in total. They take this very seriously and start really
slowly. Since you’re there all day you take things to do. We took our computers
for us, and lots of coloring things, books, iPod shows, table games, etc. to do
for Lindy. You also bring snacks and water – they want the stomach to have
something else in it besides the allergen (fruit and crackers was what we did).
The water is for squishing after each dose to make sure it doesn’t linger and
irritate the mouth.
3.
Q: Are there age requirements?
A: The only restriction is that they must be able to physically eat peanuts – so babies are out. His youngest patient was just a little over 3. Our daugther was 3.7ish years old when we started. It very much depends on how “compliant” your kid is. Will he/she take the medicine? Frankly, I was worried about our squirt on this one – still am a bit. She’s up to eating real peanuts now, but doesn’t love them, so it’s sometimes hard to get her to want to eat them (chocolate is helpful here). Dr. Jones says he thinks younger patients handle their anxiety about treatment better; it’s harder for older kids who understand that they could have a reaction to remain calm while eating peanuts. He has a lot of children and adolescents as patients, but has a growing number of young adults 18-25. His oldest patient is a 65 year old physician who has had many anaphylactic episodes during his life and he’s ready to be done worrying about it! Everything seems to be working the same for him as for the kids!
A: The only restriction is that they must be able to physically eat peanuts – so babies are out. His youngest patient was just a little over 3. Our daugther was 3.7ish years old when we started. It very much depends on how “compliant” your kid is. Will he/she take the medicine? Frankly, I was worried about our squirt on this one – still am a bit. She’s up to eating real peanuts now, but doesn’t love them, so it’s sometimes hard to get her to want to eat them (chocolate is helpful here). Dr. Jones says he thinks younger patients handle their anxiety about treatment better; it’s harder for older kids who understand that they could have a reaction to remain calm while eating peanuts. He has a lot of children and adolescents as patients, but has a growing number of young adults 18-25. His oldest patient is a 65 year old physician who has had many anaphylactic episodes during his life and he’s ready to be done worrying about it! Everything seems to be working the same for him as for the kids!
4.
Q: What if my allergy is worse than yours? Is it
safe?
A: You can see our girl’s blood work on this post.
She’s anaphylactically allergic to the 3 peanut proteins. However, she has
never reacted to anything processed in a factory that processes peanuts or
reacted to the smell of peanuts in a room, so I’m sure there are kids who are
more sensitive than she is. However, it is those super sensitive kids who need
this treatment the most, since completely avoiding a peanut particle floating
in the air for the rest of their lives is very unlikely! We’ve heard other
parents say that their doctors do not recommend this treatment. But I think
they need to think about the source of that information for a second. While I’m
sure that they care about your child as a patient, they also aren’t likely to
recommend you leave their office to be treated somewhere else (can you say “conflict
of interest?”). They might say, “It’s not safe!” And that’s true – it isn’t
safe to do it in THEIR office – they do not have the protocols in place, nor
the experience needed to offer this program safely. Dr. Jones does! They are
ready for the worst. If someone were to have an anaphylactic episode in the
office, they are prepared to intubate and stabilize before rushing over to
Davis hospital which is a parking lot away. They have never had to do that.
They have had to give their cocktail of antihistamines (described in the next
post), and they have had to do epinephrine injections, but they’ve never had to
intubate. Even those who had reactions continued on, and have “graduated” the
program. I know we sound like we’ve been paid to advertise for him, but the
results advertise for themselves! My anaphylactically allergic kid is eating
peanuts! Our old allergist would never have been able to do that for us. For
those who have been told not to try this treatment, please at least talk to Dr.
Jones, go to one of his seminars, or check out the news reports – it can’t hurt.
There are kids who have had serious reactions in the past who have graduated or
who are currently in this program – you are not alone!
5.
Q: How can they do this so quickly? Do they do
this for seasonal allergies?
A: I’m not sure how the biology works, but
something about actually ingesting the allergen and building up the tolerance
that way is actually quite fast. In fact other allergens can be treated even
faster! The milk allergy program is done in 4 months (I think), while peanut
takes 6. But still… 6 months of weekly visits for a lifetime of freedom… um…
YES! For seasonal allergies they do allergy shots just like other offices. I’m
guessing the time frame and treatment plan will differ from person to person,
and I don’t know if it’s any quicker at his office than any other. We have
seasonal allergies, but are attacking the peanut at the moment.
6.
Q: Does insurance cover it?
A: This probably depends on your insurance company.
We have Select Health and immunology is covered once we hit our deductible.
However, you will want to double check with your insurance company to make sure
RMAAI (aka. Dr. Douglas Jones) is covered by your plan. Before treatment begins
they will get all your insurance information and determine how everything will
be paid – they want to make sure they get paid, just like any other business.
So if your insurance company doesn’t cover this, I’m pretty sure you’ll find
out early on. Billing happens once a month even though you are incurring costs
every week. They are billed like a
normal physician office visit in our case.
7.
Q: How can I learn more?
A: Here is a link to RMAAI website. You'll probably be interested in some of the videos on the website too if you're interested.
A: Here is a link to RMAAI website. You'll probably be interested in some of the videos on the website too if you're interested.
Tuesday, March 3, 2015
Q&A Part 1: Diagnosis and Prognosis
Prepare for a long-winded-Katie-authored post. But first a cute kid is pretty excited about her first whole peanut tomorrow!
Now that we’re about half-way through the oral immunotherapy (OIT) treatment, we thought we’d answer some of the questions we've been asked over the last few months – and hopefully now we have pretty good answers. But remember that this is our experience, our perspective, and our daughter – many things will not be exactly the same.
There’s so much to talk about, we’re going to split our Q&A into at least 3 different posts: Diagnosis & Prognosis, Dr.’s Office Questions, and Home Dosing Items. So stay tuned!
Q: "How did you even know she was allergic?"
A: Many people have asked us this question out of concern for their own babies since it never occurred to them to maybe shy away from common allergens with their kids. In case you're wondering, the 8 serious allergens are peanuts, egg, milk, shellfish, fish, tree nuts, soy, and wheat.
We already gave a short timeline of how we figured out what was going on, but here's the more detailed version for those interested.
Family History: Our kid has at least 3 cousins on her maternal side that are allergic to peanuts (and other various things... soy, milk, etc.). Their peanut allergies have not caused significant problems, and they have chosen not to do blood tests. They just avoid anything obviously peanutty. Since we knew it ran in our family, we knew it might be something to look out for.
 First Exposure: After she turned a year old (the advice at the time, and for most mainstream pediatricians, is to wait until the child is at least a year – more on this later), we gave her a peanut butter sandwich. She seemed to like it, no problem. This is how all allergies work. The first exposure doesn't cause any reaction because the body has not made any IgE antibodies against the allergen yet. The cells responsible for making the antibodies needs to "see" the allergen first, then it ramps up IgE production. Check out this site for more information on how food allergies work,
First Exposure: After she turned a year old (the advice at the time, and for most mainstream pediatricians, is to wait until the child is at least a year – more on this later), we gave her a peanut butter sandwich. She seemed to like it, no problem. This is how all allergies work. The first exposure doesn't cause any reaction because the body has not made any IgE antibodies against the allergen yet. The cells responsible for making the antibodies needs to "see" the allergen first, then it ramps up IgE production. Check out this site for more information on how food allergies work,
Second Exposure: A few days later we gave her another peanut butter sandwich. This time she didn't eat all of it, and seemed to have some red itchy looking splotches around her mouth. We thought since there was a family history of peanut allergy we would hold off on the peanuts for another year or so before trying again.
Third Exposure 18 months: While getting a treat one day as a family I unthinkingly gave her a tiny sample cup of peanut butter frozen yogurt. No red splotches this time, just a rash over her entire body! We called our ER doctor brother-in-law and he helped us find the right dose of Benadryl for someone so tiny. She seemed itchy and very crabby from what I remember. But after the Benadryl and a good nap she was fine. At this point we realized this was a real thing, and we needed to see an immunologist.
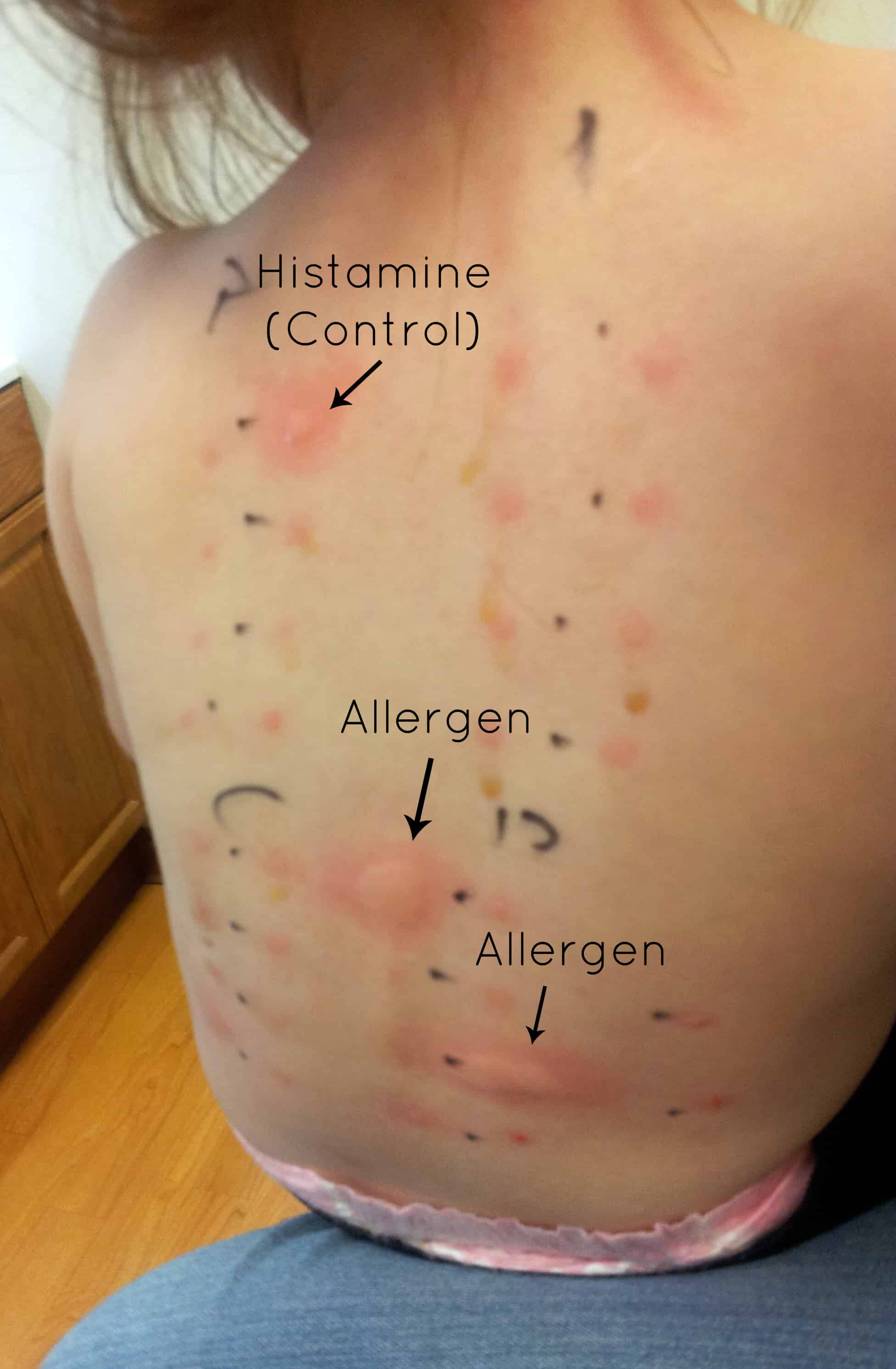 |
| Not our daugther, but similar test |
Our daughter was tested against peanuts and other nuts (tree nuts). She was 20 months old, and like any 20 month old she wiggled and squirmed and didn't like what was going on. As luck would have it, the histamine control and the peanut serum dripped down her back a little and ended up all over her arm and side. She screamed HARD for 20 minutes straight. I’d never heard her cry like that (not even with sleep training). We had to hold her arms so that she couldn't scratch anything – she was supposed to be still. We were all absolutely miserable. In retrospect, I should have realized that the part on her arm and side was not normal, and should have had the doctor apply the antihistamine cream to those areas, but I didn't, and we ended up dealing with some long-term consequences. When they finally came in to read the results, the peanut serum had dribbled into the space for almonds, so the Dr. wanted to repeat the test. Um… no way! Instead I suggested that we do the blood test for almond antibodies since we were doing one for the peanut antibody anyway (DUH!). All the other nuts were clear. They finally put the anti-histamine cream on her little tortured back, arm, and side and she fell asleep in my arms almost instantly, completely exhausted. Previously she handled vaccinations and well check visits pretty well, with the normal baby/toddler cry for a minute, then get over it attitude. After the back scratch test, she started crying the second a doctor tried to listen to her heart, refused to stand on the scale just to get weighed, and wailed if any sort of medical instrument was brought within close vicinity. After talking to some other moms at RMAA, I learned that this may have been an abnormal situation – it didn't sound like their kids had been as traumatized.
Blood Tests: Next up we had her blood drawn (another traumatic experience, but it had to be done). Turns out that it was just that the peanut serum did in fact get out of its prescribed circle – she is not allergic to any other nut but peanuts. We do not know if she’s allergic to anything else, as we didn’t have any other immediate concerns and her back was too small to try much else other than nuts at the time. I have absolutely no desire to ever have her do a back scratch test again, but we will likely have to do blood draws every now and then (every 6 months according to this first allergist – haven’t asked the second). The results of her blood tests were described in a previous post, but the take away is that her allergy was getting worse (even with decreased exposure) and that we needed to be prepared for a “very bad” reaction should she ever ingest a peanut – so keep her away from them. Period.
Ever since then, we have been a peanut free home (if only we were allergic to sugar and fat). I haven’t missed it as much as I thought I would – but we’ll both be very happy to have peanut butter cookies again, granola bars, trail mix, Rees’ Peanut Butter Cups………
Q: What is the prognosis for someone with a food allergy?
A: Again, I’m going to be specific to peanut allergies, because that’s what we can speak to. Of all the food allergies, peanuts are the most common cause of food-induced anaphylaxis and hospitalizations. Anaphylaxis is when multiple body systems are responding to the allergen – so you might have any combination of throwing up, rashes/hives, drop in blood pressure, and airway swelling. It’s this airway swelling and drop in blood pressure that are most scary as a person having a reaction can no longer breathe and if not treated right away, can die. If a severe reaction takes place, you treat it with epinephrine. These reactions can occur minutes after exposure, so it is important to have epinephrine with the person who’s allergic at all times – there may be absolutely no time to wait for the paramedics!
 Lindy should have her “Epi-Pen” with her wherever she goes. If we go to the store, we have it (at least in the car). If she’s being babysat, the sitter will get a lesson on how to use the autoinjector. When she’s playing at a friend’s house, her medicine bag goes with her. She has it at preschool. She has it at grandma’s house. She has it with her at all times. We have never had to use it, thankfully, but we try to make sure everyone is prepared should she ever need it. For more information on the “Auvi-Q” epinephrine autoinjector that we use, check out their site. It’s pretty cool!
Lindy should have her “Epi-Pen” with her wherever she goes. If we go to the store, we have it (at least in the car). If she’s being babysat, the sitter will get a lesson on how to use the autoinjector. When she’s playing at a friend’s house, her medicine bag goes with her. She has it at preschool. She has it at grandma’s house. She has it with her at all times. We have never had to use it, thankfully, but we try to make sure everyone is prepared should she ever need it. For more information on the “Auvi-Q” epinephrine autoinjector that we use, check out their site. It’s pretty cool!
Recently there have been some news reports of people who died from allergy-induced anaphylaxis. It got me wondering just how common these kind of deaths are. From my brief time researching, apparently it’s hard to pin down all these allergy numbers. It might be because some people mistake an intolerance for an allergy, or because there are sometimes other factors like asthma that play a role in who reacts more severely. But I feel like it’s a question of when, (not if) Lindy will get exposed. She will. Peanuts are in a vast amount of foods, and in several things you would not automatically think contained peanuts. Here’s a list if you’re curious. That’s why we feel like this is a necessary step for her. That’s why people from around the world have moved to Layton, Utah for a few months, just to be a part of this. It feels like we’re actively diffusing a ticking time bomb! We’re so thankful!
Thursday, February 5, 2015
Peanut Flour Dosing
Since each week she goes back for an "escalation" dose of this peanut protein, and since the end-goal is for her to be eating 24 peanuts at a time to "graduate" from this program, of course that means that eventually she'd have to come off of the liquid syringe dosing and move on to something more substantial. That time has arrived:
Yes -- that's straight ground-up peanut flour in there. Yes, she's allergic to it. Yes, we feed it to her twice a day -- intentionally. Yes, she does just fine with it and we continue to progress forward.
You probably won't have a full appreciation for how wild (and relieving) it is to me that she can do so much of it so soon when we've been avoiding it so strictly for so long.
We take it out of the capsule and usually mix it with pudding. I confess that I enjoy smelling the chocolate pudding/peanut mixture. I think I'm going to get a bag of peanut butter M&M's when this is all done. And hey, she seems to enjoy it too.
No problems so far. No significant reactions. And we keep moving forward. It's very encouraging to see some major progress here.
[A big thank you to our family for helping watch the littlest kiddo at home while Katie takes her to do these escalation doses every week!]
Subscribe to:
Posts (Atom)









